Value-Based Healthcare (VBHC) in action: Key takeaways from ICHOM 2023
The ICHOM Conference 2023, the world's largest VBHC event, brought together leaders from the international public and private healthcare sector including pharma, policymakers, payers, providers, patient representatives, academia and MedTech. The conference aimed to continue building momentum for change that matters to patients, and it was a great success. We have summarised our key takeaways from the conference below.

1. VBHC adopters across the globe
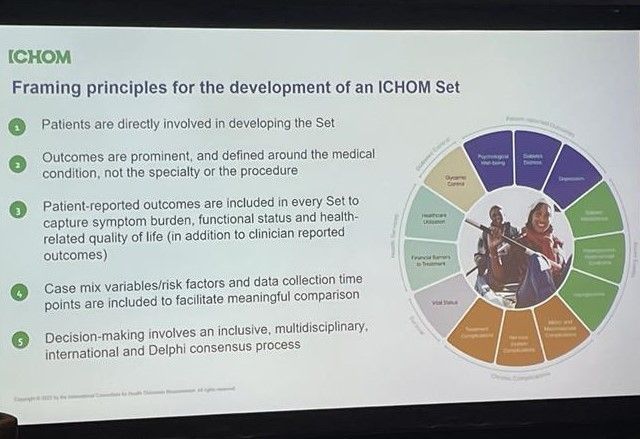
VBHC is happening across the globe. Selected healthcare providers have started to measure and improve outcomes that truly matter to patients. They are leveraging standardised approaches such as the ICHOM sets or PaRIS (patient-reported indicator surveys by OECD) for outcome collection.
They were developed in collaboration with a global expert community and patients. The ICHOM sets have been implemented in over 450 case settings across 42 countries – with Germany and the Netherlands as the leading implementation countries.
Outcomes-based agreements (OBAs link payment to achievement of treatment outcomes) have proven to be a successful tool for implementing VBHC on the pharma and payer side – who feel a responsibility for managing uncertainties and ensuring healthcare system sustainability. A global pharma company highlighted that OBAs have resulted in timely patient access, positive impact on QoL, and budget predictability. Pharma and payers emphasized the critical success factors for OBAs:
- Cross-functional collaboration within pharma
- Early and long-term stakeholder partnerships between pharma, payers, providers and patients based on trust, transparency, and common goals
- Alignment on how to measure which patient-relevant outcomes
- Data and information sharing
2. Remaining challenges for VBHC adoption
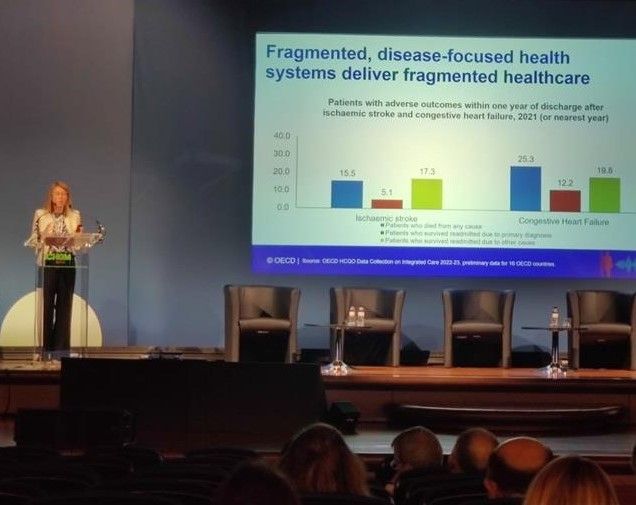
VBHC leads to increased efficiency, better resource allocation, and improved patient outcomes than the traditional fee-for-service care models which are characterized by a lack of outcome measures to optimize treatment based on the patient’s needs and preferences. Still, key challenges remain for VBHC adoption.
Limited awareness of VBHC
Different stakeholders including the public, policymakers and patients have often limited awareness and understanding of VBHC. This limited VBHC literacy has effects. For instance, it can limit policymakers’ willingness to prioritize VBHC on the political agenda.
Limited trust among stakeholders
Pharma, payers, providers and patients explained that there is usually limited trust between stakeholders to collaborate and share outcomes data (PROMs & CROMs). This hinders intersectoral collaboration, cross-sectoral expertise, and successful OBAs. One of the key reasons mentioned for the limited trust is conflicts of interest between various stakeholders.
Healthcare systems under pressure
In settings where outcomes are measured, they are often not comparable because measurement standards are not followed or implemented uniformly. This makes it difficult to use the outcomes data for benchmarking, identifying innovators, improving quality of care at large scale, and supporting policy-making.
3. Solutions to drive VBHC adoption
The challenges presented in adopting VBHC call for concerted efforts from all stakeholders in the healthcare ecosystem. To make VBHC a reality at large scale and reap its benefits, the following actions are imperative:
Developing VBHC educational campaigns
Stakeholders need to be educated on the importance of VBHC, the patient perspective, and the role of data in improving patient outcomes and quality of care. Patient advocacy groups emphasized that VBHC literacy campaigns for the public and policymakers should leverage patient stories:
VBHC literacy campaigns should also emphasize the importance of institutionalizing patient involvement in health policy decisions:
Educational campaigns should train healthcare providers on collecting and evaluating PROMs and CROMs in a standardized manner (e.g., following the ICHOM sets). These different campaigns can help to create a VBHC mindset and shift the cultural paradigm among policymakers and healthcare providers. Once providers and policymakers adopt a VBHC mindset, their commitment, conviction, and leadership are required to implement VBHC.
Building trust among stakeholders
Transparency and data quality emerged as the key drivers for trust-building during the conference. While pharma should openly communicate the knowns and unknowns of their products (e.g., real-world effectiveness and budget impact), patients should be given access to their data. Multiple stakeholders highlighted the need for information sharing and an open dialogue to make VBHC work. The trust issue can be overcome with strong stakeholder partnerships and joint initiatives based on common goals and transparency. Trust-building between providers and patients is also considered crucial for enhancing shared decision-making and supporting personalized care.
Healthcare systems need to be strengthened to respond to the patient voice – ICHOM is currently developing a Patient Charter that patients and healthcare systems can leverage.
The panel discussions also revealed that healthcare resources should be optimized by directing them towards collecting PROMs (i.e., using patient surveys as diagnostic tools) and improving patient-relevant outcomes. Pharma and providers highlighted that providers need to be incentivised to collect PROMs in a standardized way through compensation that correlates with outcomes. The standardized approach towards PROMs and CROMs collection allows for benchmarking of outcomes which can inform decision-making at different levels. Providers also need better clarity on how the outcomes are integrated into the regular care pathway (e.g., to inform treatment choice). Ultimately, providers that deliver better patient outcomes at competitive costs (e.g., through preventing hospitalization) thrive in VBHC.
Consensus also exists that integrated and secured digital infrastructures are essential for VBHC to work. But remember:
4. Best practices
Inspirational initiatives of early adopters to showcase VBHC as a solution to current healthcare challenges:
- The transformation of Saudi Arabia’s healthcare system, moving from an institution-centric towards a patient-centric approach, is a clear example of a country embracing a VBHC mindset. They aim for an integrated healthcare system where cost and outcomes are continuously measured.
- The Hospital Clinic Barcelona is adopting the VBHC model and implementing the ICHOM sets (for inflammatory arthritis, age-related macular degeneration, hip prostheses, knee prostheses, liver oncology, and upper limb surgery). The quality management team developed tools to collect and integrate PROMs and CROMs and conduct a cost-effectiveness analysis of the different treatment options.
- The GluCare Integrated Diabetes Center in Dubai integrates a patient-centric approach with technology to deliver healthcare following the VBHC approach and ICHOM diabetes set. The centre leverages digital platforms to streamline care delivery for diabetes patients.
- The Michigan Surgical Quality Collaborative (MSQC) supported by the American Blue Cross, has brought together hospitals, clinicians, and researchers to improve surgical outcomes. They share data and best practices, and work collectively to enhance patient care. The initiative has resulted in avoided complications, reduced length of stay and cost savings.
- The European Society of Cataract and Refractive Surgeons (ESCRS) Registries provide a model of data-sharing platforms. With more than 3 million records collected from 16 countries, the ESCRS Registries are among the most prominent projects in ophthalmology. These registries help track the outcomes and experiences of patients undergoing eye surgery.
Nominated research projects at ICHOM 2023: Winner of VBHC Prize 2023, Winner of NEJM Catalyst price 2023